Left heart failure (mechanism and symptom): Definition
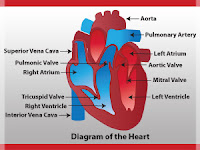
See also heart failure (advice), bloodstream. Synonym: heart failure inability of the heart, specifically the left one (left ventricle) to perform its function of the pump to propel blood. Heart failure affects about 1% of the population age 50 and 10% after 80 years an estimated 17 million people worldwide suffering from chronic heart failure. More, for instance, chronic heart failures is defined as a set of complex symptoms that occur during a period in which the heart cannot assume a cardiac output (amount of blood ejected minimum) sufficient and necessary to the normal needs of all the body tissues. More precisely it is the ventricles (left and right) that ensure the ejection of blood from the heart. The blood circulates in a closed circuit in the blood vessels, arranged in two vascular loops: the systemic circulation that distributes blood to organs and tissues and the small circulation which feeds exclusively lungs. The heart is located between these two systems, will serve as the engine of the circulatory system, it divides it into two parts, a left heart and right heart.
The left heart receives oxygenated blood (or arterial) from the small circulation and blows it into the aorta is the largest artery in the body. The aorta is somehow a starting point of the general circulation, which is the main artery. It carries blood to the organs by successive ramifications. Recent arteries called arterioles (arteries microscopic) finally distribute blood to the deeper tissues (all cells constituting an organ). These arteries possess elasticity, which allows them to reduce fluctuations in blood pressure. They will regulate the pressure inside the artery and arteriole each, to avoid the excesses that can lead to cardiovascular disease.
Capillaries to arterioles follow that release oxygen to the cells and recover their waste. Then the blood, loaded with toxins from the cells, follows the path of return, using channels increasingly important: first venules and veins and venous trunks finally to eventual reach the vena cava (upper and below). These veins are very flexible and oval shaped. On the other hand, within their wall is not smooth, it is made of folds shaped nest of pigeons: the valves. These valves are designed to prevent blood from flowing back into the cells where it comes from.
Finally, venous blood enters the right heart. Then he left the high traffic for small circulation towards the lungs. Leaving the right heart, it happens in the arteries and arterioles and ends in the pulmonary capillaries. Once in the lungs, it discharges toxins that it has cleared the cells and oxygen due to the presence of air in the alveoli. It can then go back to the left heart, having grown from venous blood than in arterial blood. To return to its starting point, that is to say, the left heart, he borrows the pulmonary veins that do end up in the left atrium. From there, through the mitral valve, it enters the left ventricle and goes finally to the organs through the systemic circulation.
Causes
In general, heart failure is a complication of heart disease. We must distinguish the right heart failure of left heart failure. It left ventricular failure is likely to be complicated by right ventricular failure creating congestive heart failure.
Left heart failure, left ventricular may be due to (non exhaustive list):
A rise in blood pressure
A valve damage such as shrinking
Aortic valve insufficiency or mitral
Heart disease of congenital origin (aortic coarctation corresponding to the narrow isthmus of the aorta)
Ischemic heart disease type, that is to say, characterized by a reduction or cessation of blood flow in one or more arteries of the heart.
Cardiomyopathy, that is to say, a disease of the heart muscle itself
Endocrine disorders (hyperthyroidism excess secretion of thyroid hormones)
Rhythm disorder
Symptoms Asthenia (fatigue) in the effort
Tachycardia
Tachypnea (high respiratory rate) greater than 20 breaths per minute at rest
Dyspnea: difficulty breathing during an effort (Shortness of breath)
Dyspnea at rest with choking sensation when the patient is lying down and falling when getting up or sitting.
Dyspnea occurring at night so sometimes accompanied by paroxysmal cough and expectoration of pink color announcing the acute pulmonary edema and corresponding to the most dramatic manifestation of left heart failure and liver damage.
If shortness of breath occurs at night and is associated with bronchial spasms it is probably difficult to distinguish cardiac asthma with bronchial asthma itself.
The auscultation of the heart can highlight what is called apical corresponding to the beats of the heart within the chest located to the left and down.
It also allows you to hear the famous gallop as it is called by the specialists is likely presystolic and an accentuation of the second heart sound at the base (noise lung). The auscultation of the lungs itself suggests the moist rales containing bubbles at both lungs bases back and sides.
Additional tests and especially the electrocardiogram shows that there is an increase in volume (hypertrophy) of the left ventricle associated with bundle branch block (stop the passage of nerve impulses). Cardiologist, this electrocardiogram revealed a T wave distorted and associated with alterations due to treatment with digitalis or hypokalemia (low potassium levels in the blood).
The continuous Holter highlights arrhythmias. Premature ventricular complexes and ventricular tachycardia are not a good prognosis.
Echocardiography objective of increasing volume and left ventricular dilatation and poor contractility of it called hypokinesia and is more common when there is a lesion of the coronary arteries are the arteries for irrigation infarction, that is to say, the heart muscle itself. Sometimes, there is an effusion (fluid collection) pericardial (effusion inside the protective membranes and recovery of heart) and a myopathy (muscle disease of the heart) hypertrophic or failure (characterized by an increase in volumes and congestion).
The chest radiograph shows a heart in general increased volume and increased volume associated with dilatation of the left side of the heart. The radiologist is also shown on chest X-rays, radiological signs that is typical lung Kerley B lines. It s' is a term used by the British in 1933 Peter Kerley characterizing fine opacities appear as small white lines sometimes seen on chest radiograph's disease. There are four types.
The isotope ventriculography ejection, that is to say, the amount that is ejected from the left ventricle with each beat (systole) it is also the name of (FECG). Ejection fraction is typically 60 to 75%. When there is a malfunction of the contraction of the left ventricle ejection fraction less than 40%. In heart failure very important, ejection fraction may be less than 30% or less.
The perfusion of the myocardium is sometimes required by some medical teams to highlight cardiac myocardial ischemia (insufficient blood supply to the heart muscle).
The dosage of A-type natriuretic peptide (atrial) and type B is particularly important when there is poorer ventricular function. Natriuretic peptide BNP has also called diagnostic and prognostic value at a time. Indeed, if the symptoms are in favor of an eventual heart failure, specifically during physical examination are not always sufficient to validate and to confirm or exclude the disease. On the other hand, the additional tests described above are not regularly obtained quickly, this is why the arrival biology natriuretic peptide represents a considerable diagnostic value, especially in an emergency. Natriuretic peptide type B corresponds to a cardiac hormone (sort of neurological hormone secreted by the heart) produced almost exclusively by the right ventricle and the left ventricle.
The natriuretic peptide increases as volume overload (cardiac volume of the bracket and the increased pressure to fill the ventricles. Other words the amount of natriuretic peptides in the blood at the same time believed that the amount of penetrating blood within the ventricles and therefore, feeling. In heart failure teaming difficulty's ejection from the ventricle natriuretic peptide is likely to rise dramatically and exceed thresholds 1000 picogram per milliliter. This is not the case when it is diastolic malfunction, that is to say, the feeling of the ventricles. In this case BNP assays are between 500 and 1000 by picogram milliliter.
The second interest natriuretic peptide is to allow to distinguish between the two diseases may be mistaken (always in the context of a possible heart disease). If we take the example of acute pulmonary or lung disease in the elderly that they are like heart failure causing acute dyspnea or respiratory distress, it is now possible, thanks to the determination of this molecule to move forward with certainty the diagnosis of heart failure. Finally, the diagnostic value of natriuretic peptide is not only because this molecule also has a prognostic value. Once measured, the treatment is prescribed interval very accurate and heart failure, BNP, natriuretic peptide will enable an evaluation of this treatment.
The determination of C-reactive protein (CRP) more recently, also in the context of biological assays as well allowed to ask the diagnosis and prognosis of heart failure.
Urinalysis objective sometimes a decrease of the amount thereof (oliguria) and the presence of proteins.
Updated October 2003
The use of magnetic resonance imaging (MRI) is now part of the additional tests necessary to highlight and monitor the volume increase (hypertrophy) of the myocardium (heart muscle itself). MRI provides data complementary to the Doppler objective that the overall volume of the heart (heart weight). On the other hand, The MRI is particularly efficient, which also allows to analyze cardiac contractions is to say more precisely the mechanical function of the left ventricle.
Alerts: If you want to know more fresh update helpful articles enter your email address below and be notified by mail.